The Taubman Institute is pleased to announce a call for new applications for the Taubman Institute Innovation Program (TIIP). The institute seeks to support scientific teams which that propose focused research projects intended to impact on our understanding of human health and disease.
The Taubman institute has developed a results-oriented approach to identifying, supporting and accelerating discovery projects with the potential to become self-sustaining and to positively affect the lives of patients and their families. Since 2017, Taubman-supported projects have attracted more than $60 million in external funding following initial investment through TIIP funding.
We have no set budget and no set timeline; we want your best ideas! We are willing to take risks for potentially impactful projects.
Some of the types of studies we will consider include:
- Systematic, multi-scale phenotyping (molecular, clinical device/wearable, etc) to gain insights into individual subject variation in the susceptibility, progression, course or outcomes of disease
- Development of new devices for diagnostics, tissue sampling
- Discovery related to the underlying cause of disease
- Novel approaches to prevent or treat rare diseases
- Computational tools, machine learning, and AI approaches to understand disease
We encourage teams to include physician-scientists as leaders or contributors to the projects.
In general, we do not support animal studies, nor will we provide funds to create specialty clinics.
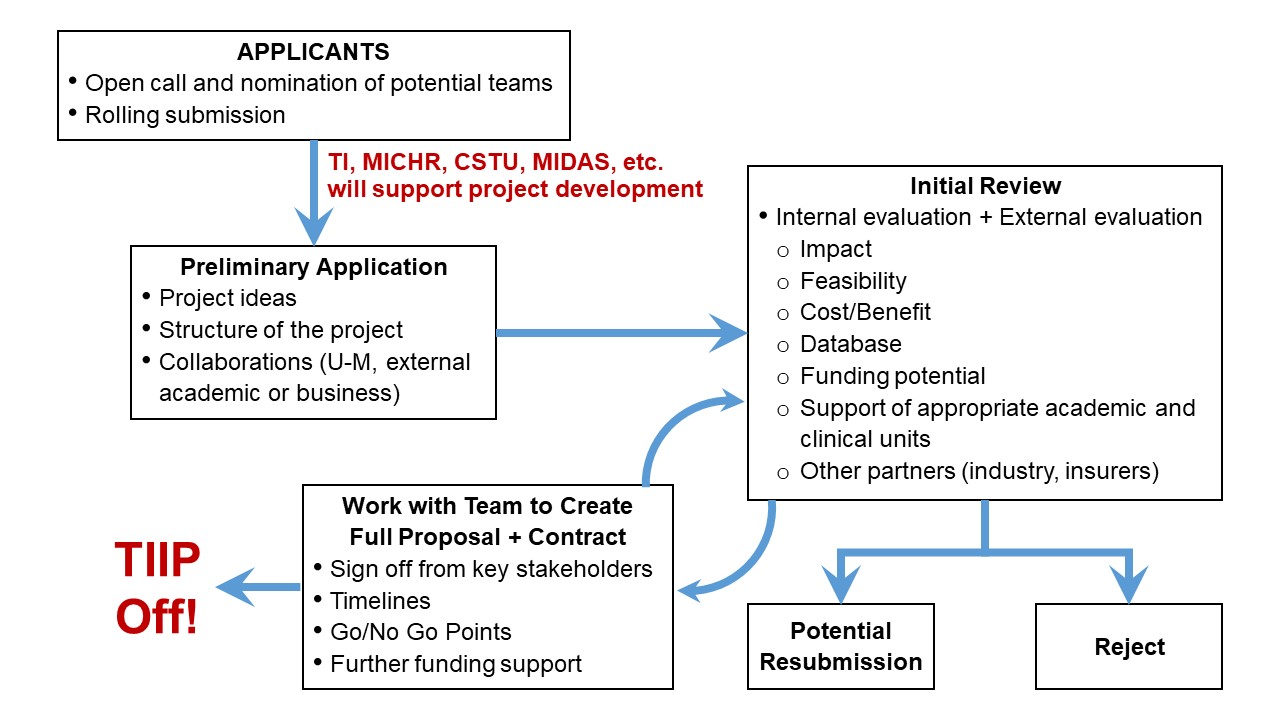
The TI approach: The institute partners with investigators to support the development and implementation of their research programs. This includes, but is not limited to, development of a research plan, database development and analysis, identification of research partners within and external to U-M, infrastructure development, support for ancillary personnel in the clinic, clinical data collection, biological specimen collection, remote data collection, initiation of research plan, and data analysis.
In addition to funding, the Taubman institute offers expertise in finance, trained project and data management, and other administrative support.
Milestones. All projects will be required to develop milestones in consultation with the institute. Continued funding is dependent on achieving the mutually agree upon milestones. Projects will undergo rigorous, periodic review by the institute’s staff, executive committee and scientific advisory board.
Who you are. The Taubman Institute welcomes applications from existing teams of active collaborators, newly formed teams, or from individuals who have novel ideas.
Funding criteria. Applications will be evaluated on the following:
- Impact on improving the lives of patients
- Innovation in understanding the variability of onset or progression of disease, and reasons for differential response to treatment
- Potential for future funding by the NIH or other external agencies
- Potential for increased reimbursement for care by insurance companies, or cost savings to the medical system
- Enhanced interactions with basic or other science disciplines (teams)
Your application: The first step in a TIIP application is to submit a letter of intent to the institute’s managing director, Grace Wu (glwu@med.umich.edu). The 2-3 page letter should include:
- A description of the proposed program
- A list of team members and their roles (please include biosketches). Describe prior interactions among the team
- What infrastructure you’ll need to accomplish the goals
- Who you’ll need to partner with to succeed
- Potential barriers to your success
Note: not all the above points must be addressed in the LOI. We seek to understand your vision for bringing science into the clinic. The main request here is for an outline of what you want to do and why it will be impactful.
Successful applicants will be expected to participate as members of the Taubman Institute community via chalk talks, symposia, public outreach events and other activities as requested by the director.
There is no deadline. Letters of intent are accepted on a rolling basis.
Next steps. Your application will be reviewed by the Taubman Institute’s director, managing director and executive committee, with feedback provided as soon as feasible.
Meanwhile, we encourage questions. You may contact us with written queries through Grace Wu (glwu@umich.edu). We are happy to meet with individuals or teams to discuss ideas.
Thank you for your interest in partnering with the Taubman Institute Innovation Program.